Plantar Fasciitis: Precision, Modality, and Measured Outcomes
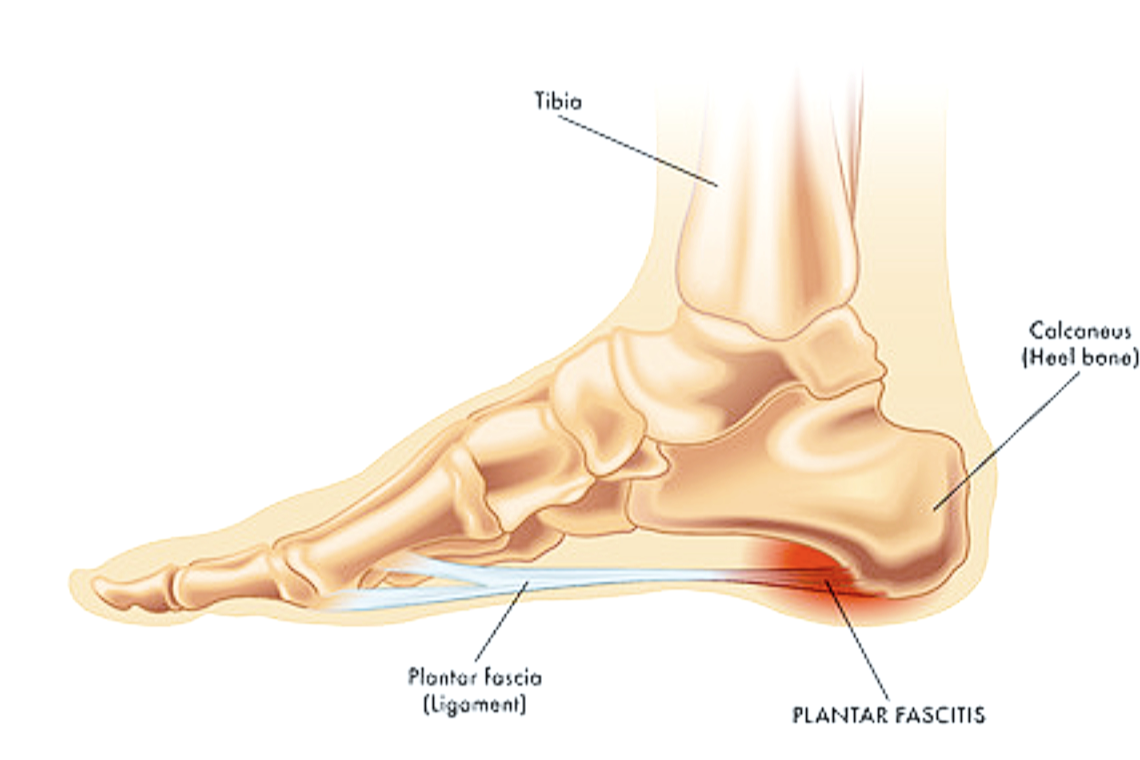
/Plantar fasciitis is a leading cause of heel pain, affecting up to 10% of the population at some point in their lives. It typically presents with focal tenderness at the medial calcaneal tubercle and pain on first steps after rest. Though often self-limiting, chronic cases require a structured and evidence-informed approach.
Orthotic Treatment Modalities
Orthoses are a first-line conservative intervention. Their primary goals are to reduce strain on the plantar fascia, correct biomechanical contributors, and improve shock absorption.
Heel Cushioning: Soft heel pads or gel inserts reduce impact forces, particularly useful in acute presentations.
Medial Arch Support: Semi-rigid orthoses with medial arch support redistribute plantar pressures and reduce fascial tension. These are especially beneficial in patients with excessive pronation.
Heel Elevation: Slight heel lifts reduce dorsiflexion stress on the fascia, particularly in cases with tight gastrocnemius or Achilles involvement.
Custom orthoses may offer tailored support, but prefabricated devices often provide comparable relief at lower cost. The choice should be guided by foot morphology, activity level, and response to initial treatment.
Additinal Modalities
For persistent or severe cases, orthopaedic interventions may be considered:
Night Splints: Designed to maintain ankle dorsiflexion and stretch the plantar fascia overnight. While some patients report benefit, compliance is often poor due to discomfort.
Taping and Strapping: Techniques like low-Dye taping can provide temporary relief by supporting the arch and reducing strain.
Footwear Modification: Rocker-soled shoes and cushioned trainers can reduce heel impact and improve gait mechanics.
Shockwave Therapy
Extracorporeal shockwave therapy (ESWT) is increasingly used for chronic plantar fasciitis. It delivers high-energy acoustic waves to stimulate tissue regeneration and modulate pain.
Radial vs. Focused ESWT: Radial disperses energy broadly; focused targets deeper tissues with precision.
Protocols: Typically 3–5 sessions over several weeks, with no anaesthesia required.
Outcomes: Clinical trials show significant improvements in pain and function, often sustained for 6–12 months.
Shockwave is most effective when combined with orthotic use and a structured stretching programme.
Efficacy of Orthotic Intervention
While orthoses are widely prescribed, their efficacy is variable. Some patients experience rapid relief, while others report minimal improvement. Factors influencing outcomes include:
Duration of Symptoms: Chronic cases (>6 months) may respond less favourably to orthoses alone.
Biomechanical Complexity: Coexisting conditions like hallux valgus or limb length discrepancy may require more tailored interventions.
Compliance and Footwear: Orthoses are only effective if worn consistently and paired with appropriate footwear.
A 2024 meta-analysis published in PubMed concluded that orthoses are moderately effective in reducing pain and improving function in plantar fasciitis, but are best used as part of a multimodal strategy